Frequently Asked Questions
What problem is Unity Ambulance facing?
Since its establishment in 1967, Unity Ambulance Corp has prided itself on being a self-sustainable emergency medical service, consistently providing reliable care to the community without external funding. However, as the healthcare landscape evolves and operational costs rise, the organization is now confronting significant financial challenges that threaten its longevity and capacity to serve. To ensure that emergency medical care continues uninterrupted, Unity Ambulance Corp is actively seeking funding support to adapt to the changing demands of our community while maintaining our commitment to excellence in service.
How Did Unity Ambulance end up in this situation?
Following the 2020 COVID epidemic and closure of Unity College, Unity Ambulance went from a volunteer ambulance service to having to pay competitive rates to attract staff. As a volunteer service with “free” help, it did not need funding from the taxpayers it serves. It continued to try not to be a financial burden by tapping into a healthy reserve fund it used for purchasing ambulances and other major equipment over the years. It has been using these funds to pay more and more for staff since 2020. Those reserve funds, without additional funding, will be gone in about 12 months.
Without Action NOW (May/June 2025) Unity Ambulance WILL Close in 12 Months…
Why is it An Emergency NOW?
To continue to provide service in the next 12 months, the ambulance must continue attracting staff. Draining its reserve funds to do this assures that:
• It WILL close in about 12 months but it is hard to attract new staff to replace volunteers NOW for a service that will close soon, and
• Current staff will start looking for positions elsewhere.
• With dwindling reserve funds, a sudden need to replace an aging ambulance will become unaffordable. This replacement will be needed soon, and without reserve funds to pay for it or to leverage a bank loan, it can’t happen.
Is There a Plan to Fix This?
Yes! One for Both the Immediate, Short Term and One for the Long Term
A project involving local representatives named by the seven towns served and advised by EMS management experts, has recommended these fixes:
Short-Term Plan: With significant 2025/26 funding from the seven towns to address the financial crisis, staffing would be upgraded with full and part-time positions to reverse and stabilize staffing losses. This level of funding needs to be continued for one to two years. The Board of Unity Ambulance will be expanded with representation from all towns served to guide operations, budget, and expenses.
Long-Term Plan: The Unity Ambulance Board, with local representatives and probably other surrounding ambulance services and towns, will explore other operational models including ambulance districts and regionalizing services, and municipal/county/fire service options.
Funding the short-term plan will assure not only meeting immediate staffing needs but protecting remaining reserve funds to also do the long term planning process.
What is the Taxpayer Cost for the Immediate Short-Term Plan?
The estimated 2025/26 mill rate based cost for a taxpayer would be just under $90 to just under $265 per year for $300,000 of property valuation. The exact amount depends on the town where taxes are paid and how much of the town is covered by Unity Ambulance (in Knox and Burnham, other services cover half the town).
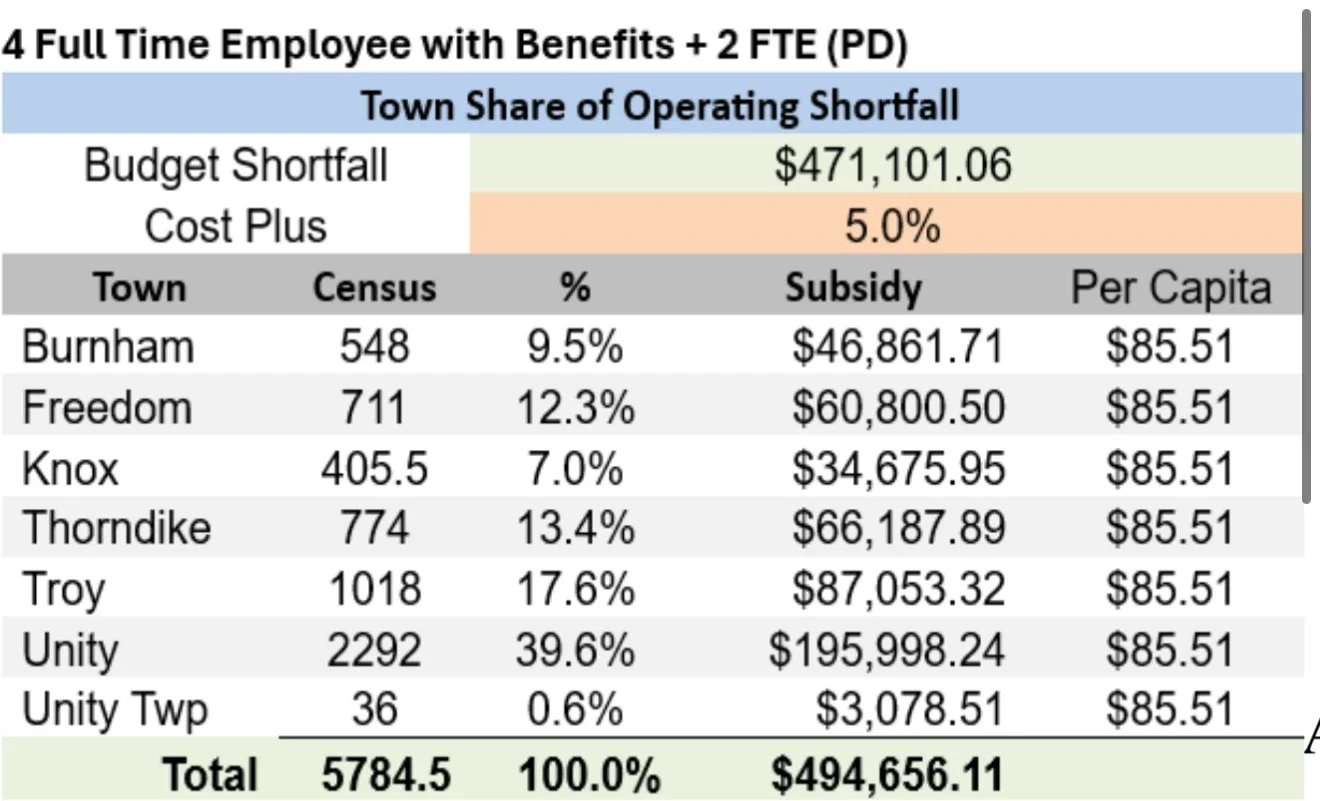
This amounts to $85.51 per capita. That is a way of comparing cost on a per resident basis not how taxpayers are charged (a four-person household is not charged 4 times $85.51 a year; the owner of the property where they live would be charged the mill rate based cost explained above).
Breakdown of costs by town:
The majority of rural Maine towns that pay for ambulance service pay about $70 to $125 per capita. The local group that created the short-term plan also looked at options that cost $55.50 or $120.94 per capita, but found them inadequate or too expensive.
What Would This Buy?
This would allow the service to hire full and part-timeprofessionals to staff an ambulance at the Unity base during the busiest times for calls most days of the week. The rest of the time, a mix of on-call, part-time and other staff would respond to calls as they most often have in the past. This will significantly reduce average response times and the frequency of “missed calls” where a mutual aid ambulance from neighboring communities would have to be called.
Would This Cost Increase Next Year?
That depends on how successful the plan is in predicting staffing costs and how unstable the economy continues to be. It would be expected that about a 3% cost of business increase might happen otherwise. After that, hopefully, the new longer-term plan would be put in operation.
Are There Any Alternatives to This Short-Term Plan?
For five of the seven towns served (Freedom, Thorndike, Troy,Unity Plt. and Unity) there really is NO BETTER ALTERNATIVE. The local steering group explored other services in the area and found Liberty and Delta (Waterville)ambulances to be the only ones suggested. Liberty charges $75 per capita which is in the same ballpark as the short-term plan cost.
The director of Delta Ambulance, now especially facing the closure of Inland Hospital, has stated that he would be extremely reluctant to offer service to even the closest towns in Unity’s response area because of staffing and other resource shortages. He also said that he could not put an ambulance and crew in Unity to serve the Unity area for less than the short-term plan’s $85 per capita.
Finally, it is a common EMS planning rule of thumb that starting a new ambulance service in an area like the Unity and surrounding towns would cost more than $1 million for 2025/26. This is twice the cost of the recommended short-term plan.
What if I Live in a Town That Funds an Ambulance Service, but I Have an Emergency in a Neighboring Town That Didn't Fund That Service?
You would receive ambulance response from whatever service that neighboring town contracts with. Towns in Maine are not required to provide or fund ambulance services. The Bangor paper reported this past January on a 9-1-1 request for EMS by a resident of a town that did not contract with any ambulance service when it was offered a contract. The 9-1-1 dispatcher was unable to find a service willing/able to respond until the ninth service that it contacted…. an hour away. The patient did not survive until that ambulance arrived.
What Happens Now and What Can I Do?
If you live in Freedom or Unity Plantation, your towns have already approved supporting the recommended short-term plan funding, so you just need to see what the results of neighboring special town meetings are in May or soon thereafter. Special Town Meetings are likely to be scheduled in the other towns in May. Check with your town office for the date, time and location of that meeting and attend it to vote your support.
Could the Town of Unity Start its Own Ambulance Service?
Again, starting a new ambulance service to serve a rural area like the seven towns served by Unity Ambulance would cost a million dollars or more in the first year. If all seven towns were asked to share the cost, it would more than double the costnow recommended by the Unity local steering group to support Unity Ambulance in 2025/26. If that service were for the town of Unity only, it would still cost in the million-dollar range, with too few ambulance calls (about 200 per year) to justify that cost.
Why is the Unity Ambulance a Separate Entity from the Town of Unity?
When the need for an ambulance service was addressed 50 years ago, the basic choice was to form an independent, non-profit volunteer service, or a service under the volunteer fire department. At the time, the independent service was chosen by those founding it and it has remained that way. Both models have been commonly used in Maine.
What Would it Look Like to be a Municipal Department?
In a town like Unity, without a town manager form of government, it would be most usual to put EMS in the local fire department, supervised by a chief. If the staff were expected to cross-train (be firefighters and EMTs/paramedics), it would be most reasonable to have all of the apparatus and living quarters in the same building, which would require an addition onto the fire station. One benefit of being a fire/rescue service is having more people at the station available to respond to fire calls, which typically require more personnel than EMS calls.
Could the Firefighters Perform Ambulance Duties and the Medical Staff Perform Firefighter Duties?
Yes, if appropriately licensed/certified per state law/rules and departmental policy. Such “cross-training” and use of each type of personnel can bring efficiencies to response. It can also discourage prospective staff hires who only want to perform one type of role and not the other. Just less than one-third of Unity Fire members are also EMS providers for Unity Ambulance. To become a Basic EMT requires a 150-hour course and passing the National Registry EMT exam. The next license level is Advanced EMT (300 hours), and the highest level is Paramedic (1800 hours). To become a structural firefighter in Maine requires a training program of at least 76 hours for Basic Fire School (not the nationally recognized Fire I/II academy), plus additional training for vehicle operators, extrication, special rescue, and leadership/instruction courses for officers.
Are Grants More Available for EMS in a Fire/Municipal Service or in an Independent Non-Profit Service?
It’s hard to say as some federal firefighting grants would not be available to municipal non-fire EMS or independent non-profit EMS. Some federal and foundation health service grants might be restricted to municipal health agencies or independent non-profit agencies. The status of these changes over time. At this moment, federal grants have been curtailed severely. No EMS agency of any type should depend on grants for operating costs, just special projects and some equipment purchasing costs.